
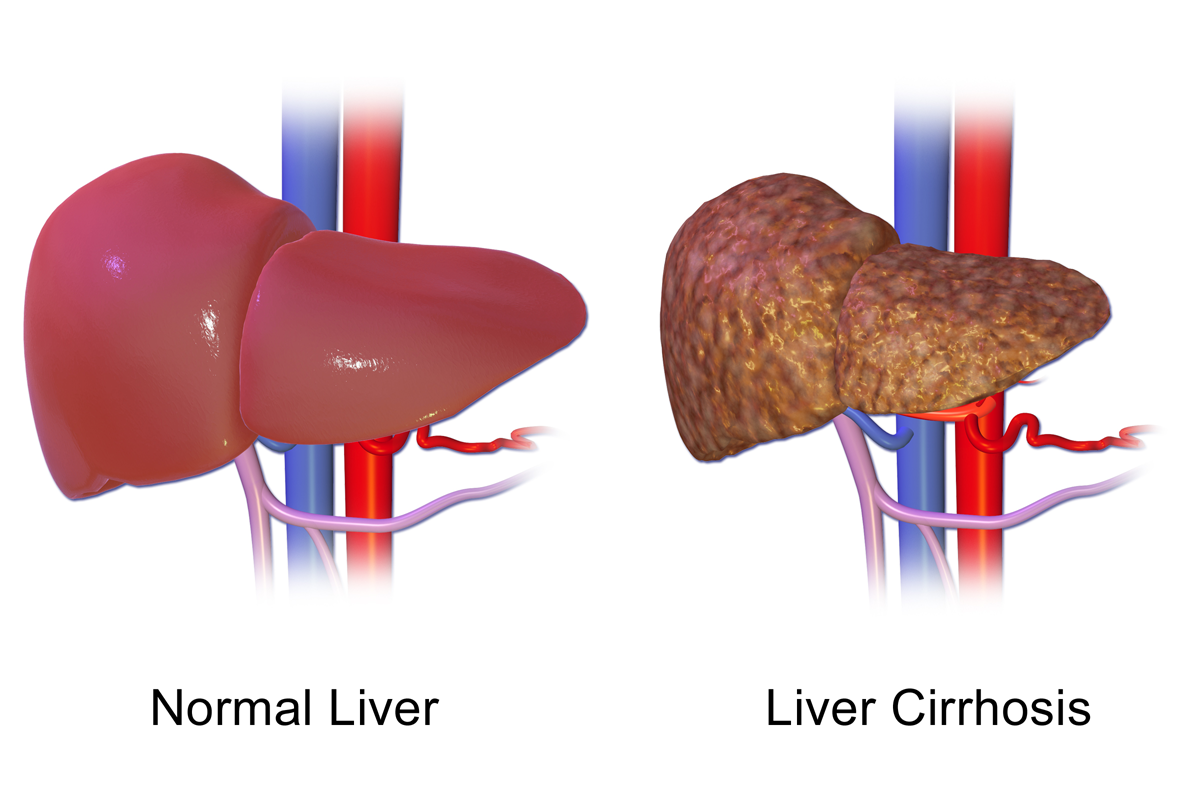
Cirrhosis means the liver is scarred beyond repair. This normally rubbery, vascular, filtration organ, the liver, becomes so scarred that it cannot carry out its duties.
In addition to not being able to perform correctly, a cirrhotic liver causes many systemic conditions and complications. Cirrhosis prevention is ideal, but aggressive management after it develops improves length and quality of life. Normally, the liver repairs damage, leaving some scar tissue each time.
Let's discuss mechanisms of damage, liver functions, altered liver functions after damage and symptoms, complications, imaging and testing, treatment, and the nursing care plan for the patient experiencing liver cirrhosis.
The liver is not easily injured, but accumulates injuries and scar tissue over a period of time via well known mechanisms of damage:
- hepatitis infection (type B or C)
- hemochromatosis (excess storage of iron)
- excess alcohol use (more than one to two drinks daily over a prolonged period)
- inherited conditions (cystic fibrosis, Alagille syndrome)
- Wilson's disease (copper accumulation)
- fat accumulation (from a poor diet with processed carbohydrates and fried foods)
- Fatty liver disease is a rapidly growing health issue and cause of liver disease in the United States.
If these damages are detected and treated early, cirrhosis may not develop. For example, an aggressively treated hepatitis infection may not result in cirrhosis. If the high iron levels from hemochromatosis are reduced (using iron chelators like Desferal), severe liver damage can be slowed or prevented. The patient with excessive alcohol or carbohydrate and fat intake may reduce liver inflammation and scarring by implementing lifestyle changes.
The liver performs many functions:
- detoxifies the body's blood (medications, alcohol, toxins)

- converts fat into energy
- releases bile for digestion
- stores excess carbohydrate for later use
- uses vitamin K to produce blood clotting proteins
- changes amino acids into energy
- converts toxic ammonia (protein byproduct) into urea
Each of these functions are altered in the chronically failing or cirrhotic liver.
- The body cannot filter medications efficiently.
- It cannot use fats correctly.
- Bleeding and bruising occur due to lack of clotting factors.
- Protein malnourishment and muscle wasting.
- Inability to clear the protein byproduct, ammonia.
- Accumulates hormones, such as estrogen.
- Fails to clear bilirubin after red blood cell breakdown.
Th
erefore, it makes sense that cirrhosis symptoms include:
- easy bleeding and bruising
- generalized pruritus
- chronic nausea and other GI symptoms
- spider angiomas
- male breast enlargement
- enlarged abdomen
- thin extremities
- cognitive issues
- jaundice
Cirrhosis complications tend to be serious, require chronic maintenance, and are occasionally life-threatening:
- Varices
- are enlarged veins, like hemorrhoids. Blood is under increased pressure, is shunted to smaller veins that enlarge, and these smaller veins become varices that can rupture. Esophageal and gastric varices are particularly dangerous and can lead to death quickly after rupture.
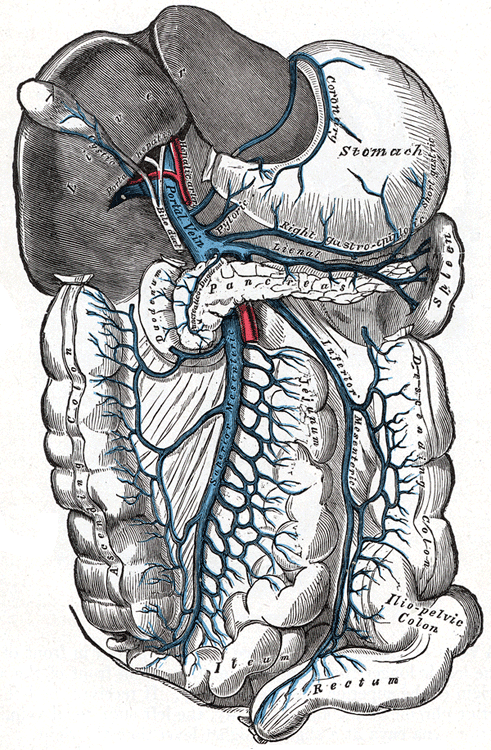
- Hypersplenism or splenomegaly
- is caused by an increase in pressure in the portal venous system within the liver (portal hypertension). The vessels are scarred and are no longer flexible, so the pressure increases. The larger spleen does not fight infection well, and, in fact, destroys needed white blood cells and platelets, instead of only destroying those due to be recycled. Infection is a further potential complication due to this.
- Pancytopenia
- a reduction in white blood cells, platelets, and red blood cells, occurs in cirrhosis for multiple reasons, one of which is an enlarged spleen caused by portal hypertension. Other reasons include changes in thrombopoietin, a hormone that stimulates red cell production; bone marrow suppression from toxins such as excessive alcohol; disseminated intravascular coagulation and hemorrhage are also potential causes.
- Hepatic encephalopathy
- occurs as a result of the liver's inability to clear toxins, like ammonia from protein breakdown. Ammonia is very toxic to the brain and causes confusion, fatigue, and can lead to coma.
- Wernicke encephalopathy
- can co-occur with cirrhosis. It is a brain damage condition caused by a vitamin B1 deficiency, frequently found in those patients with an alcohol use disorder. It also occurs in those who have malabsorption issues from other causes. Korsakoff syndrome may then develop, leading to psychosis.
- Ascites
- is fluid build up in the abdomen. Many other conditions, besides cirrhosis, can cause ascites. Amounts of up to 35 liters in the peritoneal space are possible. Portal hypertension, high pressure in the liver's venous system,
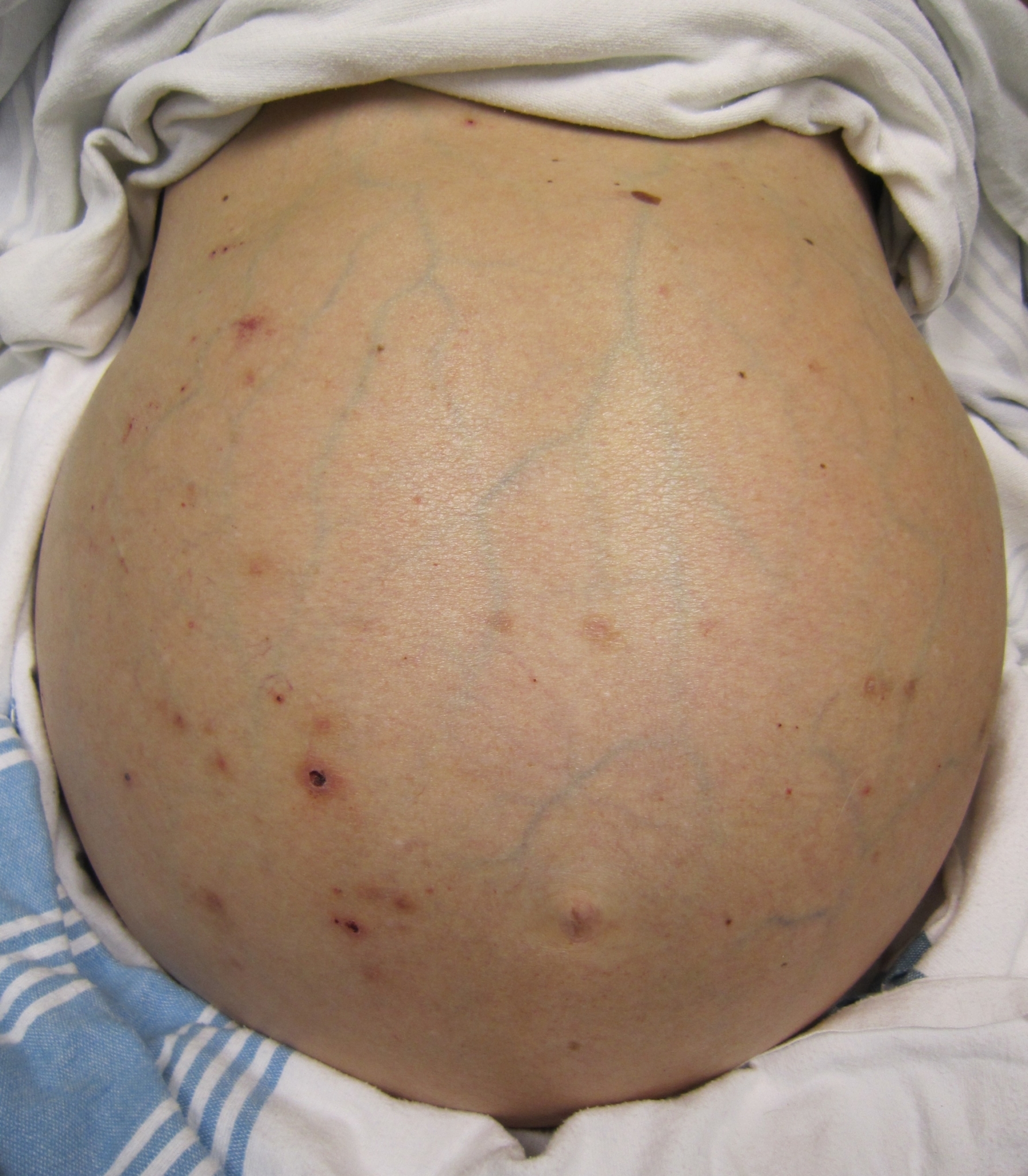 changes the capillary pressure in the capillary bed (splanchnic) within the abdomen. The elevated pressure forces protein-rich fluid out of the venous system and
into the peritoneal space.
changes the capillary pressure in the capillary bed (splanchnic) within the abdomen. The elevated pressure forces protein-rich fluid out of the venous system and
into the peritoneal space.
- is fluid build up in the abdomen. Many other conditions, besides cirrhosis, can cause ascites. Amounts of up to 35 liters in the peritoneal space are possible. Portal hypertension, high pressure in the liver's venous system,
Testing includes invasive procedures and laboratory testing of blood.
Liver function tests can be used to screen for liver problems and monitor disease progression.
- ALT and AST are liver enzymes that are released into the bloodstream due to liver damage.
- Alkaline phosphatase (alk phos) is less specific, but will also be elevated.
- Low albumin levels can indicate that the liver is not able to process proteins well.
- Bilirubin normally passess through the liver to be excreted, and it is elevated in the blood when the liver cannot process it.
- Prothrombin time is not specific to the liver, but the body can take longer to clot due to liver damage.
Imaging tests are useful to detect disease progression, complications, and other details that are useful in treatment.
- Ultrasounds detect cancer, gallstones, and liver cirrhosis.
- CT scan can demonstrate the size of the liver, fluid accumulation due to ascites, and any structures being compressed by an enlarged liver.
- Liver biopsies require special precautions to prevent bleeding in post-procedure period. A biopsy is done to get very specific liver information.

Treatment includes lifestyle changes, medical procedures, and a medication regimen.
- Performing a paracentesis can alleviate symptoms caused by an enlarged abdomen secondary to ascites by removing ascites fluid.
- An ERCP (endoscopic retrograde cholangiopancreatography) is used to diagnose, but also treat, some liver issues.
- A transjugular intrahepatic portosystemic shunt (TIPS) might be placed to relieve portal hypertension.
- Variceal band ligation is used to prevent variceal rupture, hemorrhage, and subsequent death.
- A liver transplant may be an option.
Lifestyle changes:
- No alcohol or illegal drugs
- A plant-based diet with consistent protein.
- A low sodium diet is also recommended to reduce fluid retention.
- A healthy weight
- Avoiding acetaminophen and other liver toxic medications
- For bleeding risk, vitamin K or fresh frozen plasma may be given.
- To keep systemic blood pressure low (and therefore portal blood pressure low), diuretics and beta blockers are used.
- Beta blockers are particularly important for the patient with varices.
- Octreotide (Sandostatin) is given to reduce bleeding in the case of a variceal bleeding episode.
- Chronulac (Lactulose) is given to induce diarrhea and thereby reduce ammonia levels.
- Many medications are given on a symptomatic basis such as antihistamines for generalized pruritus, antidepressants, antiemetics, and antibiotics
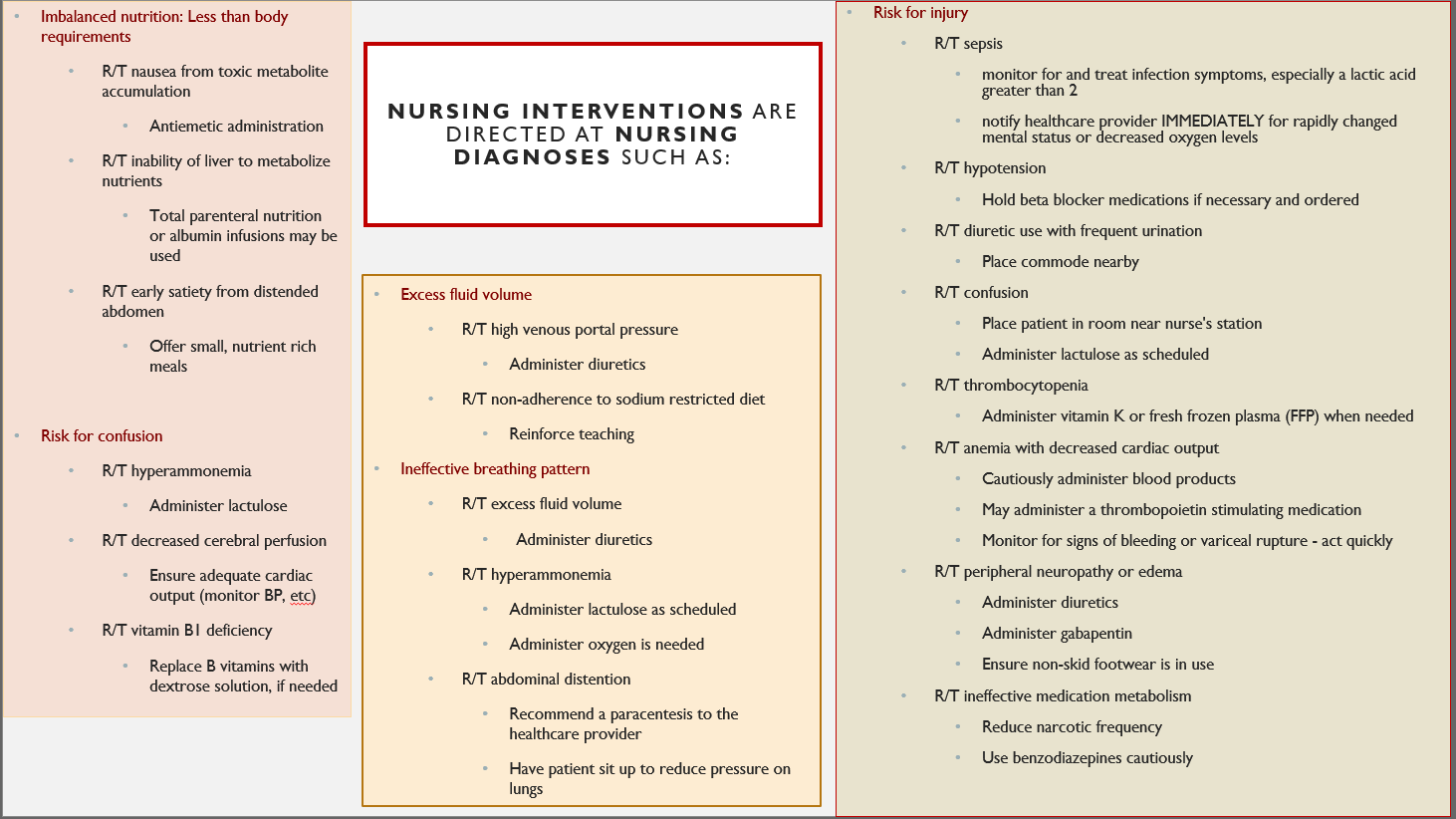
Cirrhosis care plan NCLEX MASTERY
See what folks are saying about Nursing Mastery products by HLT, like NCLEX-RN Mastery!
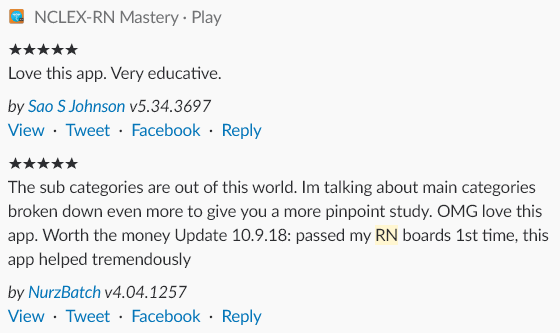
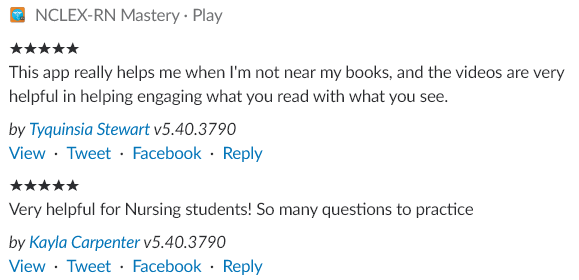
If you enjoy the free content we offer, such as this blog, let us know in the comments, on Facebook or Instagram, or by completing an app review. We would love to hear from you!!!
Resources
3D image By Polygon data is generated by Database Center for Life Science(DBCLS)[2] (Polygon data is from BodyParts3D[1]) [CC BY-SA 2.1 jp (https://creativecommons.org/licenses/by-sa/2.1/jp/deed.en)], via Wikimedia Commons
https://www.ncbi.nlm.nih.gov/p...
https://www.mayoclinic.org/dis...
https://www.ncbi.nlm.nih.gov/p...
Portal vein image by Henry Vandyke Carter [Public domain], via Wikimedia Commons
https://www.healthline.com/hea...
Image of liver venous system By Cancer Research UK (Original email from CRUK) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons; altered
https://www.quora.com/Can-you-have-cirrhosis-other-than-the-liver#
Image of cirrhosis/ascites By James Heilman, MD [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], from Wikimedia Commons
Image of normal liver versus cirrhosis By Bruce Blaus [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], from Wikimedia Commons
Fatty liver video retrieved from https://liverfoundation.org/fo...
https://www.mayoclinic.org/tes...
https://en.wikipedia.org/wiki/...
https://www.webmd.com/digestiv...
Image liver cirrhosis CT scan By Christaras A (Created from anonymized dicom image) [GFDL (http://www.gnu.org/copyleft/fdl.html), CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/) or CC BY 2.5 (https://creativecommons.org/licenses/by/2.5)], via Wikimedia Commons
https://www.mayoclinic.org/dis...
https://hcahealthcare.com/hl/?...
https://www.sages.org/publicat...
All videos are not original property and are linked to their source.



