Contrary to popular belief, cardiac rhythm identification isn't hard. What most of us need is access to a really good tutorial and lots of practice. Clinical rotations provide an excellent opportunity to get in there and look at some rhythm strips. Since we created ACLS Mastery and thought we'd share some great tips on mastering the EKG – for the NCLEX.

Grasping concepts relating to the most common rhythms is essential for today's nurse who sees sicker patients–many requiring telemetry. It is also the backbone of Advanced Cardiovascular Life Support training–a must-have for nurses interested in critical care.
The ECG represents the electrical activity occurs inside the myocardium (heart muscle). De-Mystifying rhythms begin with an understanding of the basic PQRST waveform - a graphic representation of the LUB-DUB cycle. Some simple rules about each wave tell us what the heart is physically doing. Simply-put, waves in the rhythm represent muscle contraction, and spaces between them (called intervals) represent the electrical impulse's journey through the heart...conduction pathways.
Normal Heartbeat
For basic rhythm interpretation, we can leave the Q wave out. A Q wave is the 1st downward deflection leading into the tall QRS complex and is often not seen at all. Analysis of this wave should be left for more experienced providers so we will ignore it for now.
SO, that leaves us with the following:
P wave- atrial depolarization- the atria contract, AKA:"LUB"
PR Interval - impulse traveling from SA-node through atria and AV junction (tissue between the atria and ventricles) all the way to the ventricle
This wave represents the impulse's journey from the top of the heart through the AV node and down to the Purkinje fibers along the ventricle muscle. You got it...this interval is SUPER important for rhythm analysis as you will see!
QRS complex (including the R wave) - ventricle depolarization (ventricles contract, AKA: "DUB")
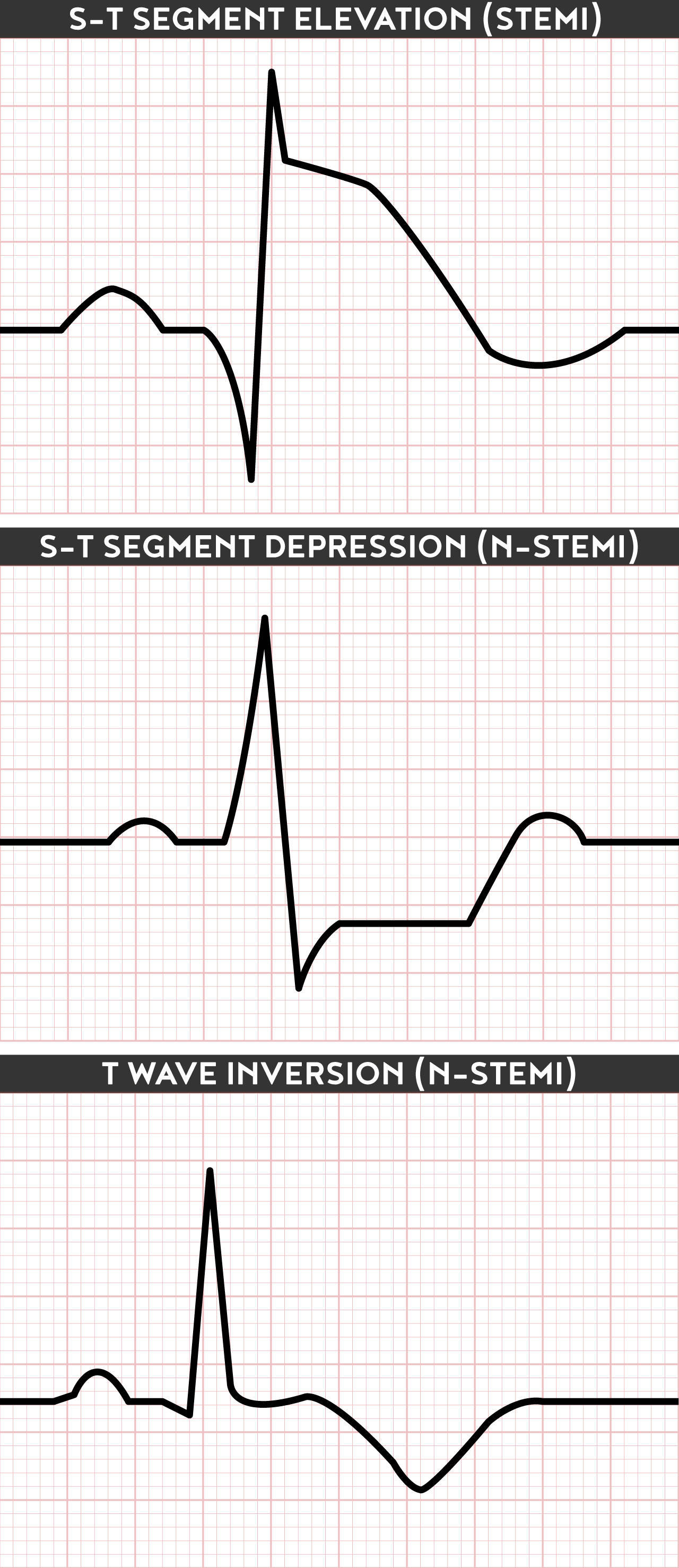
ST Interval - impulse is over, begins repolarization (rest period)
T wave - "resting muscle wave"
Once we understand what each part of the wave represents, we can apply some simple steps to analyze the rhythm...
Hint: The best lead (view) on the monitor to examine is lead II. Printing a longer strip, called a 'rhythm strip', gives the nurse enough QRS's to assess the rate and the rhythm.
Deconstructing a Rhythm
1. Look at the rate: Is it fast, normal, or slow?
2. Calculate the heart rate per minute: 6-second strip = number of QRS complexes x 10 is the easiest estimate
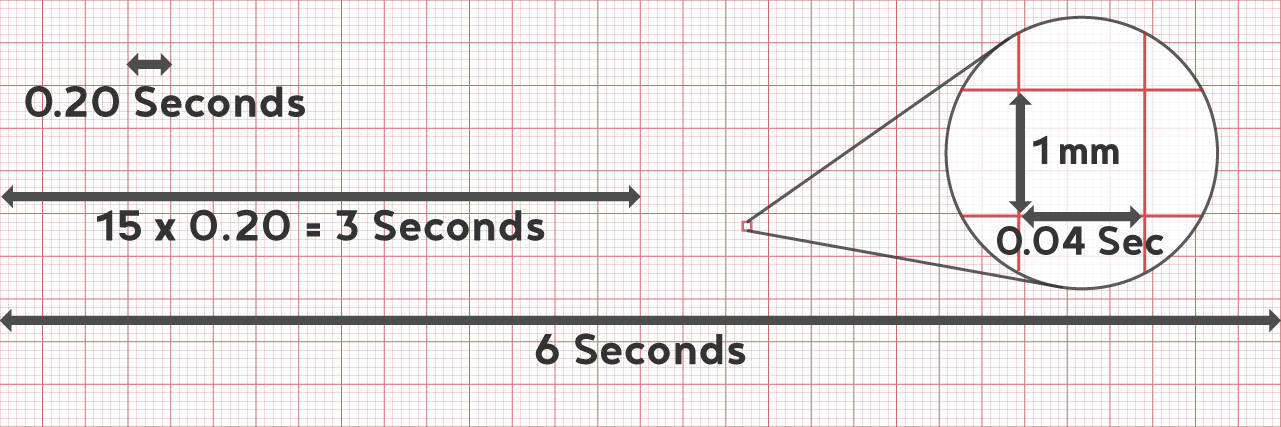
3. Determine the rhythm: Is it regular or irregular? (Measure the distance from each R-R. This distance should be constant.)
4. Examine the conduction pathways:
First: Determine what the atria are doing: Are there P waves and are they normal or inverted? The presence of P waves indicates sinus pacemaker origin. Inverted, notched, or misplaced P waves may indicate re-entry mechanisms (current traveling UP instead of down) usually from a junctional rhythm or an ectopic source. (When you see abnormally shaped P waves or those that occurring within the QRS, it is helpful to seek expert advice.)
Then: Determine what the ventricles are doing: You got it - check out that large pointed shape in the ECG zig-zag. Is the QRS waveform wide or narrow? Is it normal in shape? If it is wide, then conduction is slowed or abnormal. If it is narrow, conduction is normal or too fast.
Last (and most important): Determine the relationship between the Atria and Ventricles*: Does each P wave produce a QRS and is the PR interval constant? Are the P's farther from the QRS complex than normal? Long PR intervals and dissociated atria and ventricles indicate conduction disturbances (heart block).
One extra step: Look for possible ST-segment elevation: Take note of any obvious QRS abnormalities resulting in elevation of the ST-segment. STEMI and bundle branch diagnoses will not be discussed here, however, it is important to be aware of ST elevation myocardial infarction whenever reviewing rhythms. And always have a 12-lead ECG reviewed by a trained provider experienced in complete ECG interpretation. Nurses should be familiar with cardiac assessment including ECGs however a clinician is trained to interpret and diagnose the 12-lead reading.