Public health is a major focus of nursing practice–and for good reason. The overall strategy is simple: improve the health of an at-risk population by targeting factors that improve outcomes. Tuberculosis is a disease that all nurses learn a lot about when they prepare for licensure.
“Last year, the World Health Organization reported that 10.4 million people fell ill with TB and there were 1.8 million TB deaths in 2016, making it the top infectious killer worldwide.” ~WHO
Testing for Mycobacterium tuberculosis (TB) is an essential prevention strategy for worldwide population health. We know that TB affects certain populations more than others. TB leads all other infectious diseases in mortality, yet it is preventable and curable. Efforts to control the spread of the disease is focused on identification and early treatment of individuals at increased risk for active TB (infected individuals without symptoms, or latent infection). And now, equally important to secondary prevention, is keeping infected individuals healthy while we continue to find ways to curtail disease transmission.
Every year, heads of state from across the globe gather together to plan how to eradicate TB.
Despite decades of massive effort, TB is like many “almost eradicated” global diseases such as polio. TB strategies must address multi-drug-resistant (MDR TB) as well as HIV. The good news: TB prevention and education is cheap and fairly simple.
Get Your PPD On...Correctly
The mainstay of secondary prevention approaches is good screening processes and the standard Mantoux tuberculin skin test (TST). We will come back to screening.
To improve accuracy of interpretation, the test results should be performed by a trained healthcare professional. Nurses play a key role in performing and interpreting the test. In many facilities, standing orders allow nurses to screen clients and conduct this testing, so new nurses benefit from learning about the test.
The tuberculin skin test (TST) serves to detect the body’s immune response to the antigen. A positive result indicates a delayed-type hypersensitivity reaction due to a previous infection with M. tuberculosis. The positive reaction is caused by the release of lymphokines in the skin, which draws mononuclear cells to the area in the first 24-72 hours. Erythema and edema are caused by the increased vascular permeability from this inflammatory reaction.
The preferred method is the Mantoux test, which involves placing a small amount of tuberculin purified protein derivative (PPD) just under the skin. PPD (the substance) is readily available and inexpensive. TB screening should be targeted at high-risk groups with the purpose of offering treatment for any latent TB infection (LTBI). Although there may be occasions when low-risk groups may be targeted as well (daycares, schools), routine testing is not beneficial, as it leads to unnecessary treatments and can be costly.
Most persons can receive a TST. Mantoux testing is contraindicated only for persons who have had a severe reaction (e.g., necrosis, blistering, anaphylactic shock, or ulcerations) to a previous TST. It is not contraindicated for any other persons, including infants, children, pregnant women, persons who are HIV-infected, or persons who have been vaccinated with BCG (bacille Calmette-Guerin - a TB vaccine).
The PPD test is performed by inserting a small gauge needle intradermally on the forearm and injecting 0.1 mL of PPD solution. When the test is performed correctly, a characteristic 6 mm to 10 mm wheal forms. Then, the client waits.

Test Interpretation
Accurate interpretation (reading) of test results relies on examination of the test site no earlier than 48 hours and no later than 72 hours following placement of intradermal purified protein derivative (PPD). A trained health care professional (usually a nurse) documents any induration (swelling and/or hardening of tissue at the injection site).
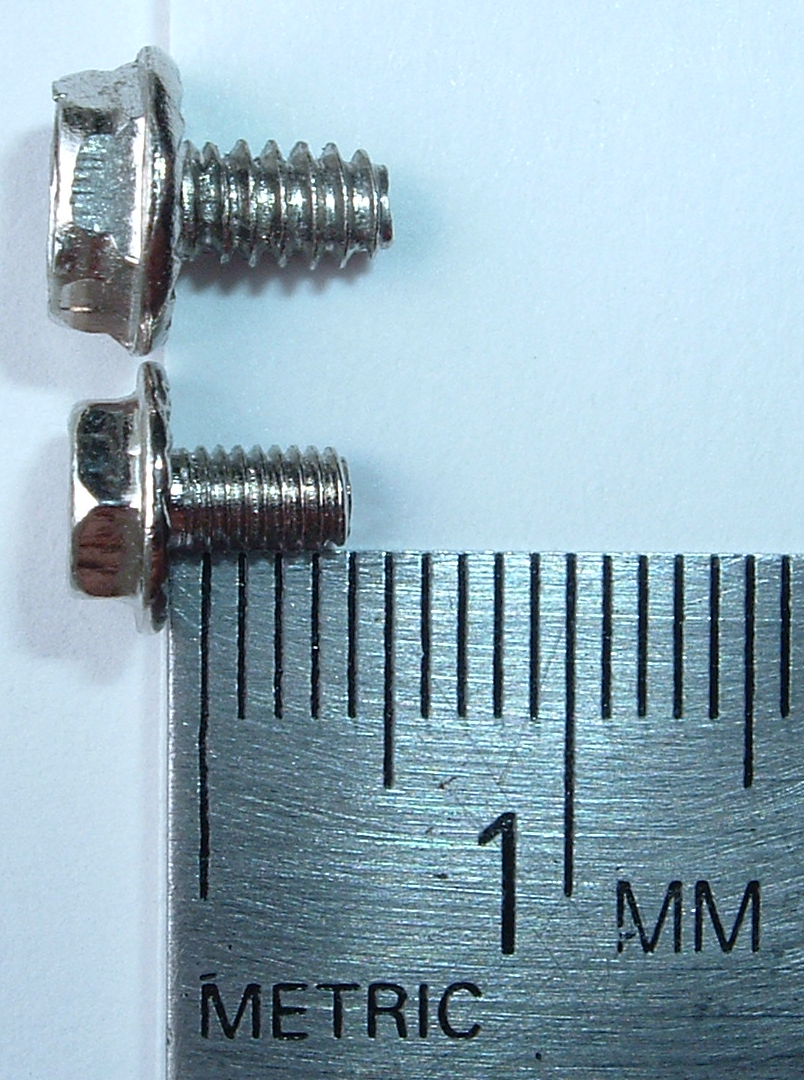
The only thing needed for test interpretation? A TB skin ruler or a ruler with millimeters for measuring induration.
Patients who do not return for reading of the TST within the 48–72-hour time period must repeat the test. A TST that was not recorded or measured by induration size in millimeters (mm) is invalid and must be repeated.
- Induration is any area of hardened tissue at the injection site. Induration may be accompanied by surrounding erythema, however TST measurement is based solely on the size of the area of induration in millimeters.
- The CDC mandates reporting of all positive TST results for investigation of exposure and transmission and prevention of future cases of TB through contact investigations. A positive TST must be reported to the appropriate public health authorities for guidance on treatment and follow up.
- Patients or family members should never interpret TST results. Most practice laws require that licensed staff perform PPD readings.
Booster Effect and Two-Step Testing
Some people infected with M. tuberculosis will have a negative reaction to the TST after many years have passed. They may have a positive reaction to a TST only after a first TST stimulates their body’s ability to react to the PPD antigen. This is referred to as the booster phenomenon. For this reason, the “two-step method” is recommended for individuals who may be tested periodically (e.g., health care workers, prison workers), to trigger any latent immune response.
If the first TST in the two-step is positive, the person is considered infected. If the first test result is negative, the TST is still repeated in 1–3 weeks. If the second test result is positive, it means the first TST activated an old immune response to his or her previous TB infection and the person is infected. Only if both steps are negative is the person considered uninfected. This is the type of testing healthcare professionals are typically asked to have done for employment.
Why screen?
Performing a Risk Assessment
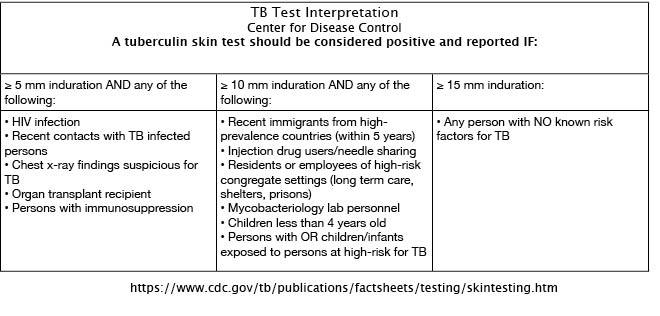
TST interpretation is based on two factors: induration measurement in millimeters and the patient’s risk factors (history of exposure/infection and risk of progression to disease). For this reason, it is best to perform testing for those at high-risk.
Non-TB mycobacteria, history of BCG vaccination, and incorrect method of TST administration or interpretation can cause false-positive reactions. It’s important for the nurse to review risk factors with patients and document the assessment.
Risk factors are used, in fact, to determine positive results…and thankfully, the CDC provides guidance...
For more information:
For TB Stats go to CDC Fact Sheet
Learn more about a TB-Free World in the CDC website
Image attributions:
CDC PPD Wheal Image Author: Greg Knobloch
Public Health Image Library image: CDC/Author: Donald Kopanoff
