On November 18, 2015, at the urging of the public and many agencies, including the Department of Health and Human Services, the U.S. FDA approved the use of naloxone nasal spray for the treatment of life-threatening opioid overdose.
The legislation that followed in most states echoed the response to recent stats showing deaths by overdose surpassed motor vehicle crashes as the leading cause of death due to injury.Narcan (naloxone) is now available to the public as part of a broader campaign to combat an opioid epidemic and is a component of the Basic Life Support (BLS) algorithm by the American Heart Association. In this article, we cover what nurses should know, including how to administer it.
Drug overdose deaths in the U.S. from the start of this century have tripled (CDC, 2016).
My wake-up call happened when I worked as a school nurse; the mother of one of my students died from methadone overdose. That came first...and then...
According to the National Survey on Drug Use and Health, prescription drug abuse is the fastest-growing drug problem in the United States. In 2015, over 6 million individuals over age 12 reported they had used prescription psychotherapeutic drugs. Over half of that group was misusing prescription pain meds, and over half of deaths from opioid overdose (OD) involved prescribed drugs.In addition to misuse of prescriptions, heroin use has increased. Almost half of all poisoning deaths involve opioid overdoses. The combination of heroin and more potent synthetic opioids, such as fentanyl, has made death from overdose more likely.
EMS staff tell me that on average they use much higher amounts of naloxone to revive opioid overdoses today than they did just 5 years ago due to these newer, stronger prescription opioids.
As nurses, we must provide appropriate pain relief, and also treat those with substance use disorders. Believe it or not, on many occasions, we will encounter both issues...for the same client!
So how do nurses help the opioid epidemic?
First and foremost, memorize and use the mantra!
“On a scale of 0 to 10, please rate your pain intensity, if 0 is no pain and 10 is the worst pain imaginable.”I recall trying to think of a different way to ask the same client that question many times during a single shift–wondering what they must think (it sounds so rehearsed!). Well, what they really think is: “You CARE.” Showing concern for a client’s pain each time you encounter them makes what we do meaningful and measurable.It’s like that over-played song on the radio. As much as you want to avoid sounding like a broken record–don’t. Accurately assessing pain is our window into the patient experience.
Recognize and consider pain as the 5th vital sign each and every day you go to work. Nurses must ensure that pain is treated aggressively. Period.
OK, next: learn all about medication misuse and who the experts are.
Identify what each client needs based on an assessment. This starts with a good understanding of pain treatment and substance use disorders–and more importantly, how the two may intersect.
Substance use disorder and pain management is a complex world, clinically speaking. Dependence can be recognized by signs and symptoms (withdrawal), which occur if the drug is discontinued. It usually takes about 3 weeks of routine use for dependence to develop. Tolerance is the need for more of the drug to feel its effects. These physiological terms should not be confused with addiction–a brain disease, which involves a lot more–behaviors for one.
Being physically dependent does not equal a substance use disorder if the client takes medications as prescribed (Brady, 2016).
Misuse is taking drugs differently than prescribed. This may include medication user errors due to not understanding instructions, but it may also include unprescribed use due to substance use disorder. Abuse refers to using a drug without a prescription, often to experience euphoric effects, despite resulting harm or risk. The terms are often used interchangeably.Further complicating our understanding are even MORE terms related to substance use!Take pseudoaddiction, for example– AKA “drug seeking behavior”. Nurses must recognize that this behavior may initially result from inadequate pain management. As a result, providers are challenged to manage pain–often without the use of opioids. (Brady, 2016).For many clients who fail to taper an opioid effectively, this is where the journey with dependency, and later, addiction begins.
Rule number 1 out of the NCLEX gate: It is important for a nurse to use the entire clinical team. New nurses learn fast that a social service professional is a great asset to any care team!
And the last essential tool in our opioid OD toolbox? Narcan.
Learn about it and teach others how to give it safely. We know it saves lives.
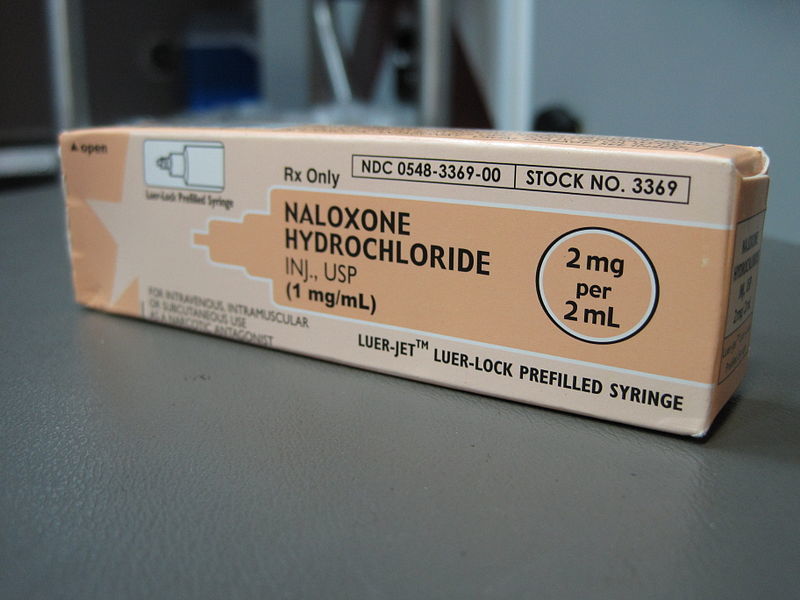
Narcan has been used in the healthcare setting for many years to treat opioid overdose–a reversible cause of cardiac arrest.
But many overdoses don't reach medical care in time. Nurses are expert teachers of health promotion and injury prevention. Raising awareness and providing education increases access for those at-risk and promotes safety. It is essential to teach clients that naloxone will not reverse the effects of other drugs including alcohol. It is strictly an opioid antagonist.States have expanded access to Narcan ‘kits’ for lay persons as part of Good Samaritan laws. These kits make it easy to give intranasal Narcan with simple instructions and pre-filled, pre-diluted devices.As part of this public health initiative, many nurses will find themselves teaching clients or family members how to administer naloxone that individuals can obtain through a “third-party prescription”. This allows a pharmacy to legally issue a prescription drug to someone other than the at-risk opioid user to keep on hand in the case of overdose.
In most states, people simply walk into a physician office or pharmacy and ask for it.
Some states have campaigned by purchasing kits in bulk and handing them out to places that encounter individuals at-risk (including hospitals).
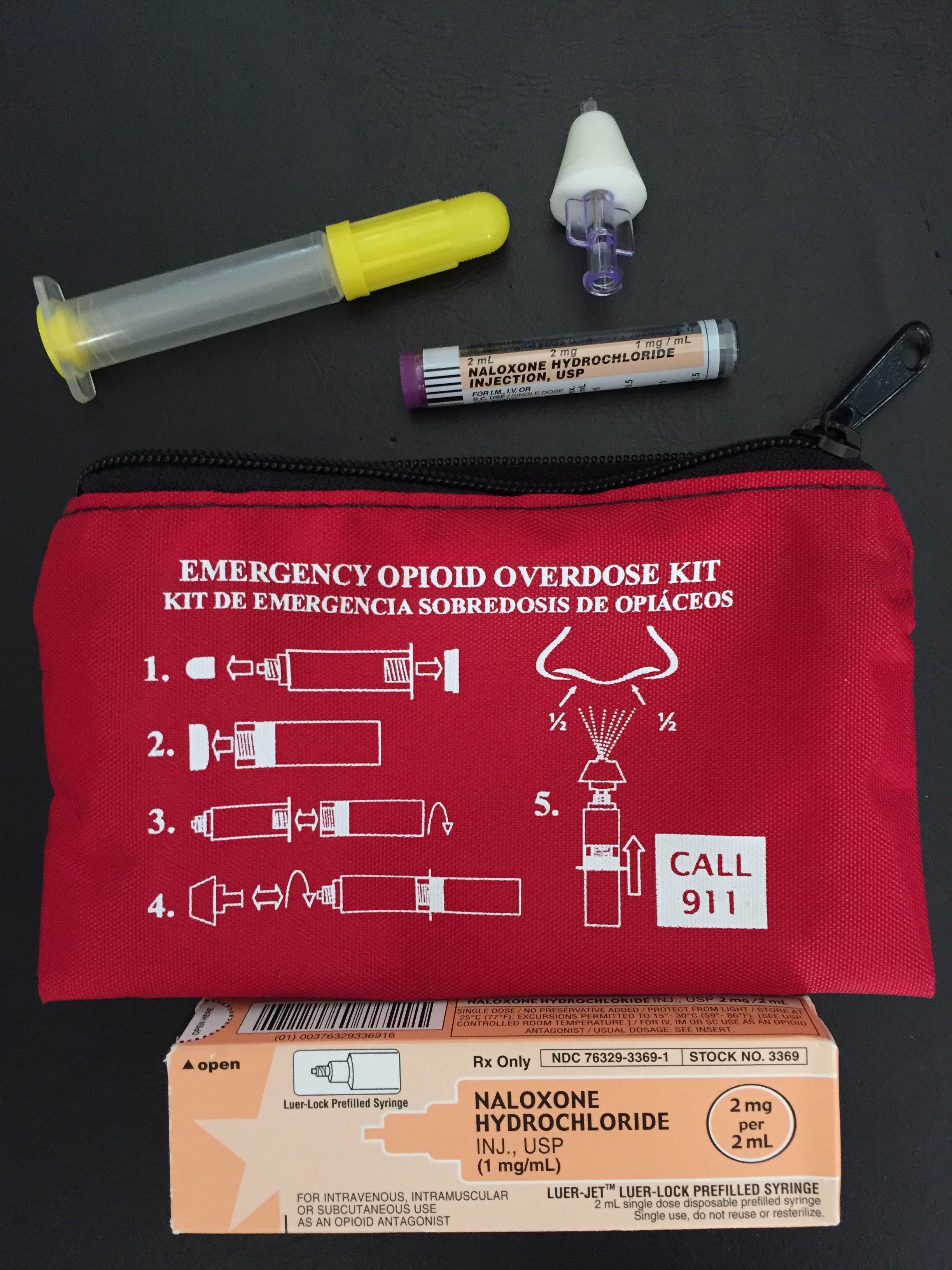
Remember, naloxone is now part of the American Heart Association’s BLS algorithm for lay rescuers to prevent or treat cardiac arrest due to opioid overdose.~Cindi Bell RN
Check out our VIDEO and LEARN MORE about this simple and valuable tool:
More Narcan Resources:
The Substance Abuse and Mental Health Services Administration offers free toolkits for opioid prevention.HHS Opioid FactsheetAmerican Heart Association CPR Highlights for Opioid Overdose EducationFor more info about opioids in clinical practice, see the CDC Guideline for Prescribing Opioids page, or contact a local government office.
Article Sources:Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51). Retrieved from http://www.samhsa.gov/data/Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65:1445–1452. DOI: http://dx.doi.org/10.15585/mmwr.mm655051e1Brady KT, McCauley, JL, Back, SE. Prescription Opioid Misuse, Abuse, and Treatment in the United States: An Update. American Journal of Psychiatry. 173:1, January 2016, p. 18-26, Print.
